Even with the rare and deadly virus that has entered our life, post-recovery, we could succumb to an equally dangerous aftereffect. Mucormycosis or black fungus affects the individual’s sinuses, brain and lungs and can be life-threatening in diabetic or severely immunocompromised individuals, such as cancer patients or people with HIV/AIDS. The drop in immunity caused by COVID-19 is said to cause this infection. It presents itself as a blackish-brown fuzzy state and grows rapidly.
To learn more about the infection TC46 connected with Dr Anita Mathew, Infectious Disease Specialist, Fortis Hospital, Mulund. Here she shares 8 signs and symptoms to monitor the infection as well as a few preventative measures.
1. Mucormycosis or black fungus is a fungal infection caused by a group of moulds
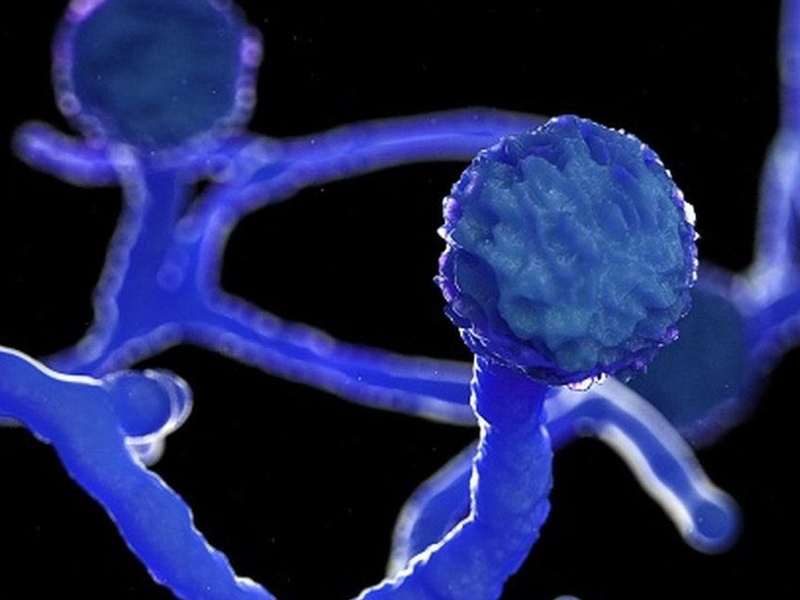
Mucormycosis is a rare fungal infection caused by a group of moulds called ‘Mucormycetes’. It is also known as the ‘Black Fungus’ as these fungi grow rapidly and have a black-brown fuzzy appearance. This infection has an overall mortality rate of 50%. The disease is often characterized by hyphae growing in and around blood vessels and can be potentially life-threatening in diabetic or severely immunocompromised individuals.
2. Mucormycosis infects parts of the body like sinuses, brain and lungs, also skin after cuts

Mucormycosis frequently infects the sinuses, brain, or lungs after inhaling fungal spores from the air. It can also occur on the skin after a cut, burn, or another type of skin injury. While infection of the oral cavity or brain is the most common forms of Mucormycosis, the fungus can also infect other areas of the body such as the Gastrointestinal Tract, skin, and other organ systems.
3. Mucormycosis can be dangerous if left untreated

Mucormycosis can be very dangerous if left untreated, it can cause mutilating damage to the face, nose, eyes with disfigurement And loss of vision, and also cause invasive brain infection. The infection causes blindness as it affects the eye through which it reaches the brain. The only option left to save the patient is to remove the affected mass through surgery.
4. Mucormycosis and COVID-19 are correlated

Mucormycosis is affecting COVID-19 patients more due to prolonged administration of steroids and subsequent immunocompromised states. COVID-19 possibly causes a change in the immune system, increasing the risk of infections in general in the post-COVID phase. To add to this, diabetes in a patient and steroid use, which if not done judiciously, will further increase the risk of Mucormycosis. Steroids reduce inflammation in the lungs caused by COVID-19 and appear to help stop some of the damage that can happen when the body’s immune system goes into overdrive to fight off Coronavirus. But they also reduce immunity and push up blood sugar levels in both Diabetics and non-Diabetic COVID patients. Therefore, the drop in immunity causes the infection. The condition presents itself with nasal blockage, blackish discoloured eyes And nose, swelling on the eye, and blurred vision. Some even come with worsened respiratory symptoms.
5. Mucormycosis appears as a blackish discolouration

- Sinusitis — nasal blockage or congestion, nasal discharge (blackish/bloody)
- Local pain on the cheekbone, one-sided facial pain, numbness or swelling
- Blackish discolouration over the bridge of nose/palate
- Loosening of teeth, jaw involvement
- Blurred or double vision with pain
- Thrombosis, necrotic skin lesion
- Chest pain, pleural effusion
- Worsening of respiratory symptoms
6. Treatment for Mucormycosis is usually surgery

Treatment is predominantly surgery to clear the virus and medicine in the form of Amphotericin B, and other antifungals like Posoconazole and Isavuconazole. Multiple surgeries are required at times for clearing the disease so that medicines can act better.
7. Curb the spread of the infection by administering the right dosage of steroids and close monitoring

The disease is not contagious. To reduce the risk of contracting COVID-19 and inhaling spores of the fungi which are in the environment, it is important to wear a mask. Keeping strict control of blood sugar (Mucormycosis even in pre-COVID times is known to affect Diabetics) is the most important thing. Judicious use of steroids would help to reduce the incidence of COVID-related mucor. One way to stem the surge of the fungal infection is to make sure that COVID-19 patients – both in treatment and after recovery, are administered the right dose and duration of steroids. It is also important that people with Diabetes, Cancer, Kidney and Liver diseases and organ transplant patients keep a check on their glucose levels from time to time.
8. Wear a mask at all times and protect your body, especially in dusty areas

Healthcare providers should keep a close watch on all our COVID patients. Especially, those with Diabetes and the ones having steroids. Use steroids of moderate quality and administer only to those who require it. Citizens should use masks if they are visiting dusty construction sites. Wear shoes, long trousers, long sleeve shirts, and gloves while handling soil (gardening), moss or manure and maintain personal hygiene, including a thorough scrub bath. The disease can be managed by controlling Diabetes, discontinuing immunomodulating drugs, reducing steroids and extensive surgical debridement – to remove all necrotic materials.

